Hip Osteoarthritis
The degree of osteoarthritis does not always determine the extent of symptoms. People may experience relatively few symptoms with substantial osteoarthritis of the hip. There may also be a lot of complaints and pain with little osteoarthritis in the hip. The degree of pain depends on many different factors such as, for example; strength of the muscles around the knee, degree of physical activity or physically demanding work. Cartilage itself has little to no pain sensors and therefore cannot cause the pain. The pain you feel is caused by an inflammatory process leading to irritation of the capsule, synovial fluid (synovium) and muscles and tendons around the knee. This is what also causes pain in osteoarthritis and therefore not the cartilage itself.
We currently have three locations. Our first physio practice is located in Tilburg Centre, at Veldhovenring 57. Our second location is located in Tilburg Reeshof, at Spaubeekstreet 89 at the Basic-Fit gym. Our third location is located in a health centre in Tilburg West, at the Professor Verbernelaan 37-D.
Cause
Exactly how osteoarthritis forms is not entirely clear. However, we do know that osteoarthritis increases with age. In this, we distinguish between different forms of osteoarthritis. Osteoarthritis can develop as a result of natural ageing. We call this degenerative osteoarthritis. Osteoarthritis can also develop as a result of an accident, which we call post-traumatic osteoarthritis. The joint is then damaged by a fall, for example. Osteoarthritis can also form as a result of an autoimmune disease such as rheumatoid arthritis (RA). In degenerative osteoarthritis and osteoarthritis due to RA, there is often osteoarthritis in several joints. Cartilage is normally a smooth structure. During ageing or damage, the quality of connective tissue decreases. As we age, cartilage cannot repair itself properly like a muscle can, for example. This is because cartilage has poor blood flow.
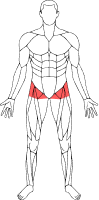
Symptoms in hip osteoarthritis
Osteoarthritis in the hip can lead to various symptoms:
- Groin pain especially after an extended period of activity.
- Clicking of the hip during flexion.
- A limitation in mobility. Especially towards stretching and turning the hip inwards.
- (Groin) pain when sitting and standing.
- Shortening of the muscles around the hip. This makes the leg appear shorter. This is not really so but is optical illusion.
Surgical intervention or conservative treatment
Surgical intervention: a new hip
When you have osteoarthritis in the hip, it does not immediately mean you need surgery. But when the symptoms only worsen and the treatments no longer have the desired effect, a hip replacement or a new hip may offer a solution. However, this choice is very person-dependent. It really depends on the perceived pain and perceived limitation in daily life. Together with an orthopaedic surgeon, the choice to replace the hip can then be made.
Conservative treatment: advice, exercise therapy and adjustments in daily life
Conservative policies focus on how to make adjustments in daily life. One example is to cycle more. Cycling is an unloaded movement. Here, there is little pressure in the hip joint but you are still moving. A structured exercise programme is drawn up where the muscles and other connective tissue around the hip are trained. Medication can possibly cause the irritation in the joint to decrease. Should this not be sufficient, a corticosteroid injection can be placed in consultation with the doctor for a local analgesic effect.
Anatomy and function of cartilage in the hip
The hip forms the connection between the femur and the pelvis. The thigh bone (femur) together with the socket of the pelvis (acetabulum) form the hip joint. Between these bone parts is cartilage that ensures that the hip can move smoothly. The hip joint is a ball and socket joint. This means that the hip naturally has a lot of freedom of movement. The hip is passively stabilised by means of ligaments. In the hip, the labrum provides additional stability. The labrum is a large, cartilage-like ring that seals the hip tightly. The labrum of the hip passes into the cartilage part of the socket of the hip. We have different types of cartilage in our body: hyaline, elastic and fibrous cartilage. Hyaline cartilage is the most common in our body and is also found on the end of our bones. In particular, the function of cartilage is to keep the joint moving smoothly and acts as a shock absorber of the hip joint. Osteoarthritis in the hip is also known as coxarthrosis in the medical world.
The different degrees of hip osteoarthritis
There are four grades of hip wear and tear, increasing in severity:
Grade I: The cartilage has softened and its springiness is reduced. Sometimes a single osteophyte (bone protrusion) is visible at the edges of the hip joint. This grade I damage is often not detectable on an X-ray.
Grade II: There are cracks and irregularities in the surface of the cartilage. However, this damage is often superficial and does not yet extend to the bone. The cartilage layer has also not yet become thinner due to the wear and tear damage. Sometimes clear osteophytes are visible on radiographs. Grade II damage is also not always detectable on X-ray.
Grade III: The aforementioned cracks have left deep grooves or holes in the cartilage. This damage extends deeper towards the bone, but the bone is often not yet exposed. However, a narrowed area of the joint is sometimes visible on the X-ray. Also, the edges of the bone ends are often affected.
Grade IV: In a grade IV lesion, the cartilage is (almost) completely gone and the underlying bone is exposed. The joint space has narrowed considerably and sometimes almost completely disappeared. Large bone protrusions have also often formed and the ends of the bone parts are deformed.
Physical tests for hip osteoarthritis
Squat test
The person stands with both feet on the ground in front of a 20-cm strip. The feet are outside the line of the strip. The person makes as deep a knee bend as possible with the hands on the hips. The heels should not come off the ground. The test stops when the person cannot lower further due to symptoms in the hip(coxarthrosis). This test is also used to assess the situation over time. A decrease in mobility probably means that the degree of coxarthrosis is increasing.
Scour test
The person lies on his or her back. The hip is flexed through the examination to 90 degrees. The knee is brought to opposite shoulder and pressure is applied towards the treatment couch. The test is positive when a recognisable groin pain is elicited.
Independent hip flexion
The person lies on his or her back on the treatment couch. The leg is brought to a neutral position. The person independently flexes the knee and hip as far as possible at that time. The test is positive with recognisable pain in the hip region. This test is also used to assess the situation over time. A decrease in mobility probably means that the degree of coxarthrosis is increasing. A well-known phenomenon during this test is a Drehmann sign. The hip will then make an outward (exorotation) movement during flexion due to the limited mobility of the joint.
Passive endorotation of the hip
The person lies on his or her stomach on the treatment couch. The knee is flexed 90 degrees. The hip is brought to maximum endorotation by the examiner. The test is positive when the endorotation is less than 25 degrees in the hip. This test can also be used to assess the situation over time. A decrease in mobility probably means that the degree of coxarthrosis is increasing.
Active extension of the hip
The person lies on the treatment couch on his or her stomach. With an extended knee, the person raises the leg as far up as possible. The front of the pelvis should remain in contact with the treatment couch. The back should also remain in a neutral position to create the cleanest possible movement in the hip joint. The test is positive with recognisable pain in the hip region.
Related complaints
Making an appointment at FysioFitaal
We work from multiple locations in Tilburg, always close by for professional and accessible physiotherapy. Fill in the contact form and we will contact you soon. Together, we will work on your recovery!

