Bursitis in the hip
Pain on the outside of the hip is a common injury. We see that it is often and quickly said that the pain is caused by bursitis, also known as bursitis in the medical world. But is this diagnosis really as common as we think? Or is it more nuanced and may other structures such as tendons or muscles play a bigger role than we suspect? In recent years, research into these complaints has yielded important new insights - insights that directly influence our diagnostics and also treatment choices. In this blog, we would like to take you through the new insights
The bursa in the hip
The term bursitis comes from Latin and partly from Greek and has two parts. The word bursa means scholarship or pouch and in anatomy refers to a fluid-filled bursa that serves as a pad between bones, muscles, tendons or the skin. The suffix -itis means inflammation and is originally from Greek. So bursitis means inflammation of a bursa.
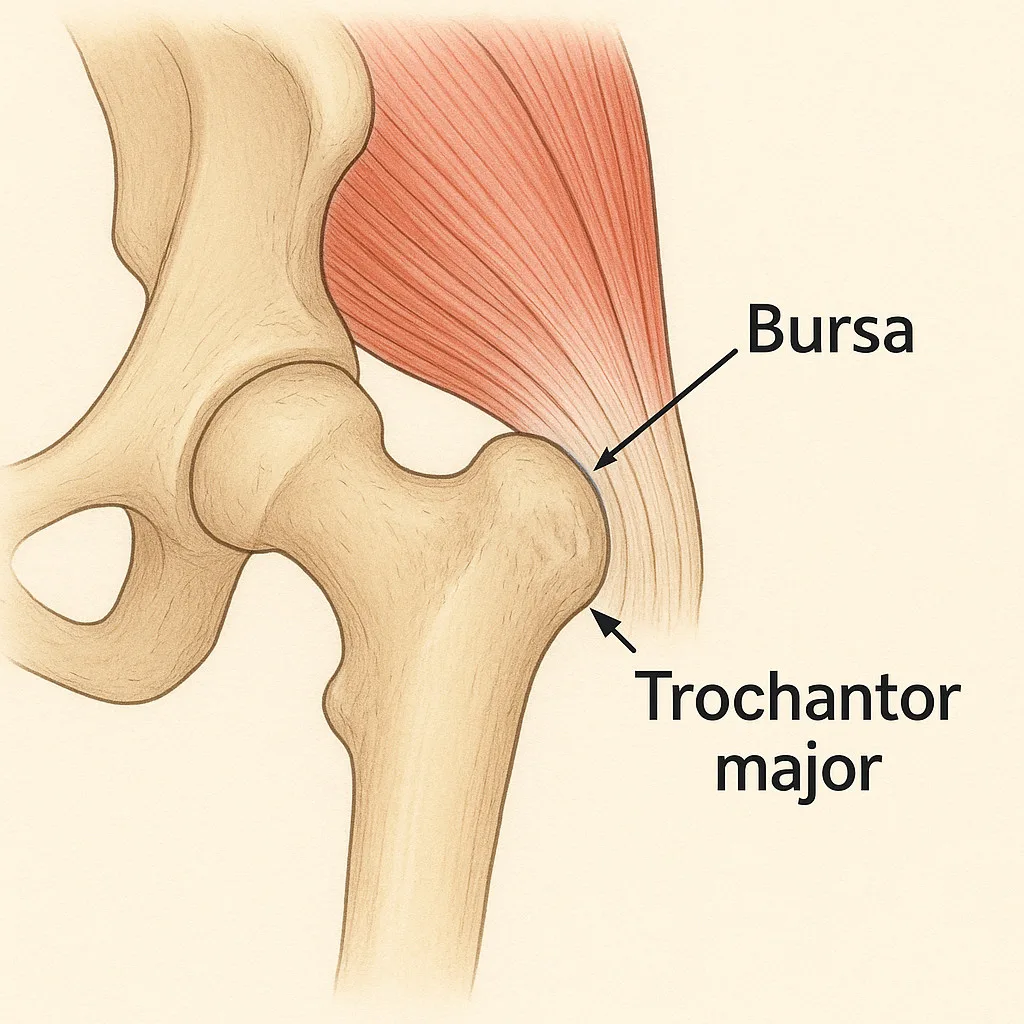
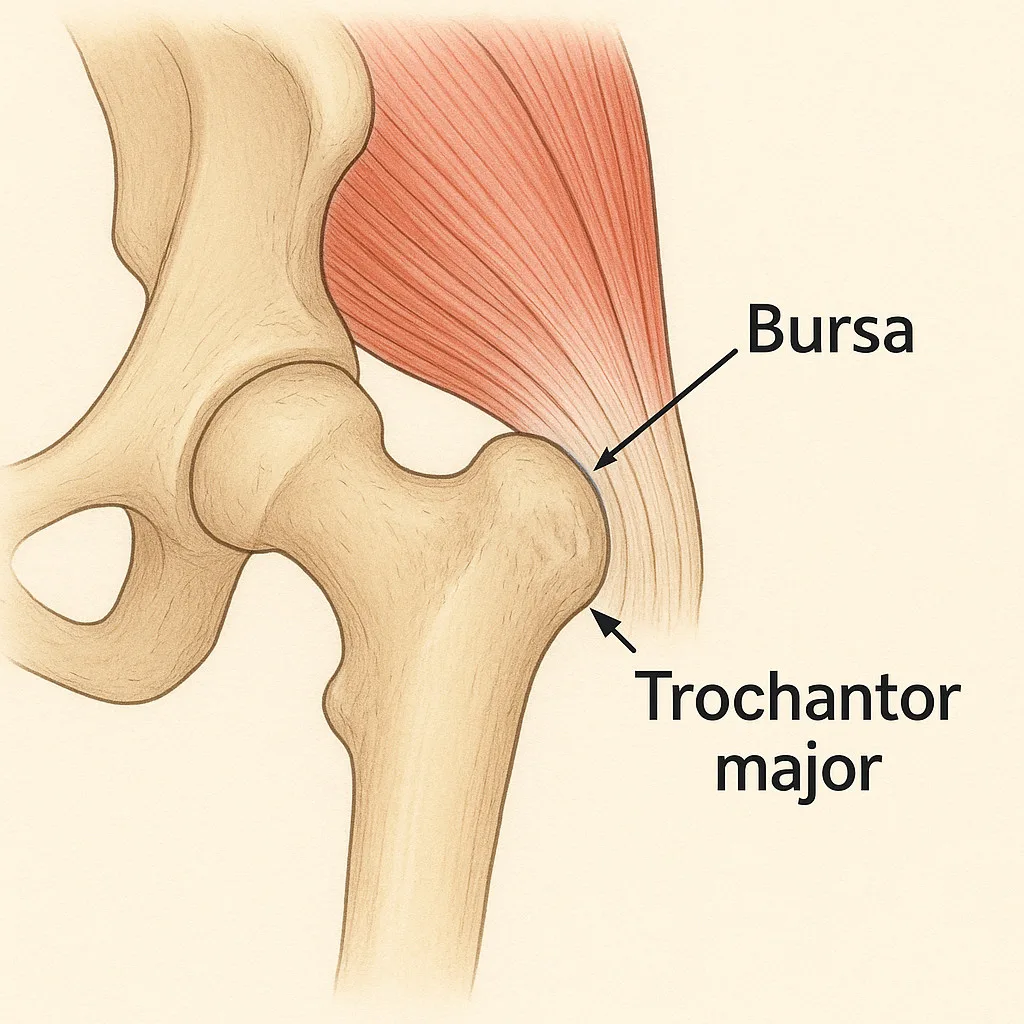
On the outside of the hip are several bursas. A bursa is a fluid-filled cushion that reduces friction between the muscles, tendons and bone. The bursa that most often causes symptoms in the hip is the bursa trochanterica. It lies between the protruding bone of the thigh (the trochanter major) and the large gluteal muscles. So when this bursa becomes irritated or inflamed, we speak of a bursitis or bursitis.
Yet in practice, it turns out that pain on the outside of the hip is not always due to bursitis alone. Often, tendon problems or other overuse problems also play a role. This is why specialists are increasingly using the broader term Greater Trochanteric Pain Syndrome (GTPS). This collective term refers to various causes of hip pain, such as bursa irritation, tendon problems, a 'clicking hip' (snapping hip) or a wrong position of the pelvis which causes extra pressure in the hip.
How often does bursitis actually occur?
A large study of people aged 50 years and older looked at the prevalence of complaints on the outside of the hip. It showed that about 15 per cent of women and 8.5 per cent of men experience this kind of hip pain (Segal et al., 2007). Often, people are then diagnosed with bursitis, but in many cases this turns out not to be true.
Studies using ultrasound or MRI show that only in about 1 in 5 cases is there really an inflamed bursa (Grimaldi et al., 2015). In most cases, the pain is actually due to a tendon problem of the gluteal muscles, also called tendinopathy. The term bursitis is then wrongly used, and this has implications for treatment, because a tendon problem requires a different approach than an inflammation.
In the Netherlands, it is estimated that 1.8 out of 1000 patients per year are diagnosed with bursitis of the hip (Nivel, 2016). But the actual rate of true bursitis is probably once much lower.
Difference in diagnosis determines treatment
It is important to know with certainty whether bursitis is present. It is therefore possible that the symptoms have a different cause. This makes a big difference to treatment, expected recovery time and advice on what activities to perform.
With true inflammation of the bursa, the emphasis is on reducing the inflammatory response. This means temporarily less stress, possibly cooling, possibly the use of anti-inflammatory medication. In some cases, a targeted injection of corticosteroids can help. The symptoms with a bursa in the hip often arise suddenly, are sharp and are located exactly in one spot that is usually sensitive to pressure, such as when lying on the side. When there is no underlying reason, bursitis usually recovers within a few weeks.
With a tendon injury, also known as tendinopathy, the approach is quite different. Then there is no inflammation, but reduced quality or overuse of the tendon. This then often involves the gluteus medius or minimus. In that case, treatment revolves around gradually building up load, targeted muscle strengthening. Although injections of corticosteroids are frequently used in hip pain, they are not a wise first choice in tendon complaints. They can worsen the quality of tendon tissue in the long term and actually delay natural recovery. Exercise therapy does work here, especially if it focuses on controlled and eccentric muscle loading around the hip. But this is not a quick fix. Exercise therapy will have to be done for a longer time to get effect. But this is the most durable solution for these complaints.
So a misdiagnosis can quickly lead to the wrong approach. Those who wrongly use the term bursitis without looking at the strain on the tendons only treat the symptoms and not the cause. As a result, the symptoms may recur more often.
Bursitis or tendon problem? Ultrasound provides clarity
Although physical examination often provides a lot of information already, the results in hip pain are not always clear or objective. Pain when pressing on the side of the hip, lying on the painful side or eliciting the recognisable pain on physical examination can occur with bursitis as well as a tendon problem. At Fysio Fitaal in Tilburg, we therefore combine the examination with ultrasound to get a fuller picture of what is going on.
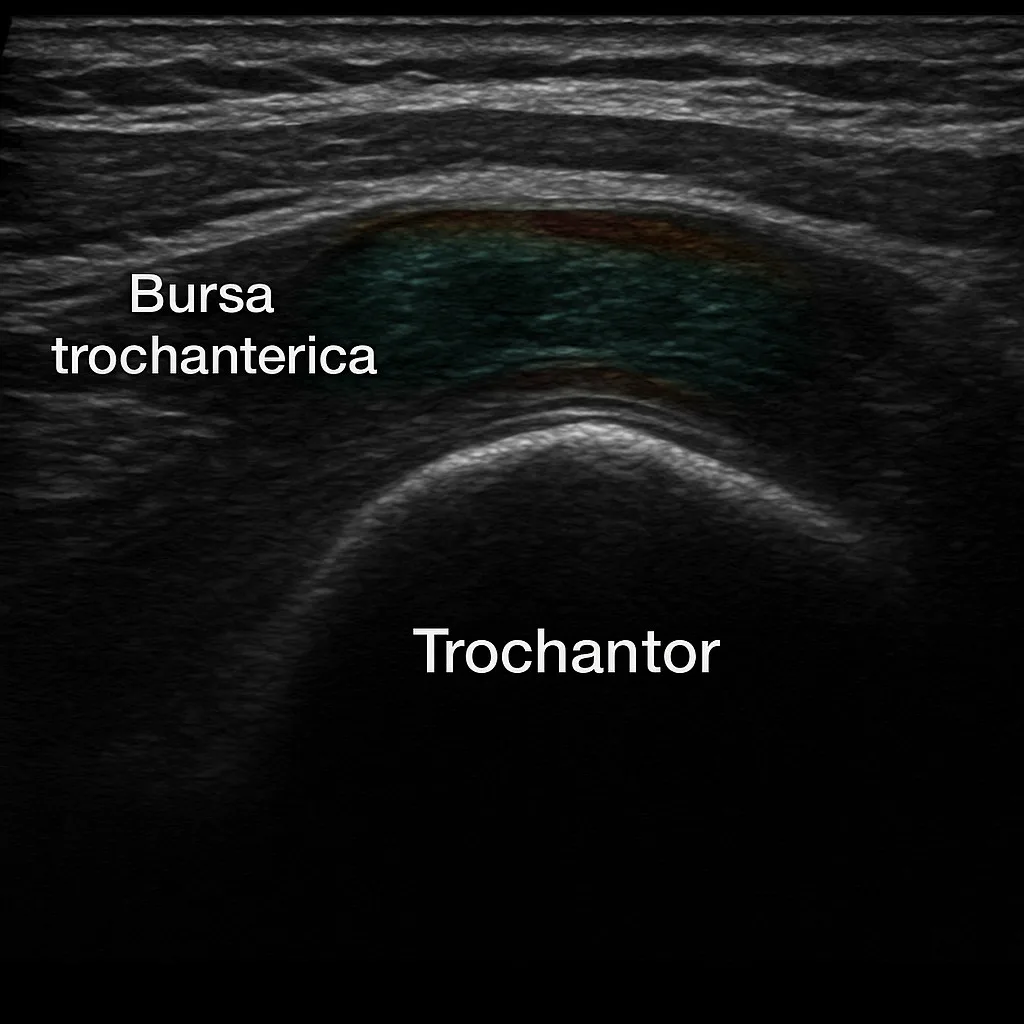
Ultrasound proves to be of great value in complaints on the outside of the hip. It makes it possible to visualise fluid in the bursa, as well as detect thickening, calcium, tears or reduced quality of the tendons. Moreover, dynamic examination allows us to see whether certain movements actually trigger pain.
A study (Kandemir et al., 2021) shows that ultrasound has high accuracy in detecting bursitis. It is a safe and accessible tool to reach a correct diagnosis.
When bursitis is actually present and an injection of anti-inflammatory drugs is considered, ultrasound can also add value here. By administering the injection under ultrasound guidance, the drug has a much more localised effect. This increases the effect of the treatment and prevents damage to surrounding tissue. Should your GP wish to have an injection administered, at Fysio Fitaal in Tilburg we can perform this together with our ultrasound technicians, so you can be assured of a safe and targeted approach.
Faster recovery with the right approach
Bursitis has really taken root in our healthcare landscape. But hip pain is often more complex than we think. Most cases involve secondary bursitis or gluteal tendinopathy without any inflammation of the bursa.
The consequences are unnecessary and annoying. Wrong treatment, frustration in the person but also caregiver. And in some cases really unnecessary prolonged complaints. A good history, targeted physical examination combined with imaging such as ultrasound are essential to prevent this.
Correct differential diagnosis between bursitis and tendinopathy not only ensures more effective therapy, but also greater understanding and a more lasting outcome!

Related complaints
Hip Osteoarthritis
During ageing or damage, the quality of connective tissue decreases. As we age...